Tick Bite SOS
Ticks in Australia- A Growing Health Concern
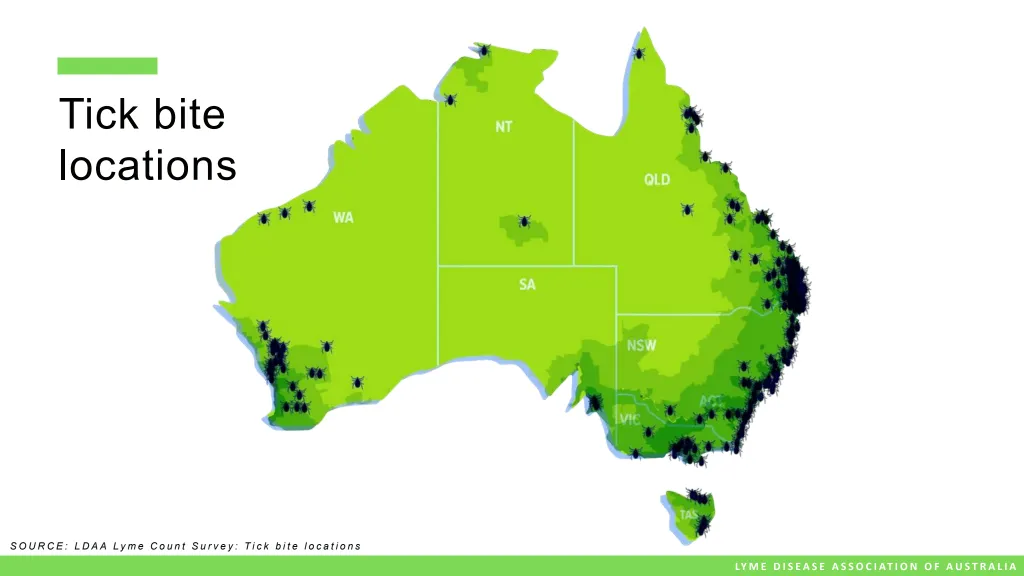
Tick bites are on the rise across the east Coast of Australia — not just in number, but in severity. Regions that were once tick-free are now seeing regular infestations, and people are experiencing stronger, more frequent reactions.
I moved to Bega shire, south NSW in 2021. Since then, I’ve had total 11 new tick bites. Nine of them led to infections, and one nearly killed me due to neurotoxin released from inappropriate removal.
This experience pushed me to dig deep into the tick issue—how to avoid them, treat bites properly, and help others do the same. I’ve been supporting locals with tick bites ever since. I’ve seen everything from mild reactions to really serious ones. You quickly learn what works and what doesn’t.
The primary species of concern in this region is Ixodes holocyclus, commonly referred to as the paralysis tick. This tick is capable of causing severe allergic reactions, paralysis, and infections in both humans and animals.
Locals say tick bites used to be a summer problem. Now it’s year-round. Even horses and livestock are reacting badly to bites, which wasn’t happening before.
I also spoke with Yuin Elders about the growing tick issue. They told me that in the past, regular bush backburns helped keep insect numbers down. They also used natural tick prevention—like crushed tea tree leaves—to keep them away.
Bottom line? Tick bites are on the rise, and they’re a real health threat. It’s time we all took them seriously.
High Risks and Misinformation
If you live in or travel through tick endemic areas and come into contact with grassy areas (even a backyard or park) the risk of getting a tick bite is really HIGH.
Safe tick removal is crucial to preventing adverse reactions.
Unfortunately, much of the advice online is based on US tick species and is NOT applicable to Australian ticks. The Ixodes holocyclus species has the longest mouthparts among ticks, embedding deeply into the skin—making removal more complex and dangerous.
Local medical practitioners often lack in-depth knowledge of tick bite managemnt and consequences.
Misdiagnosis—or no diagnosis—can lead to preventable chronic illness.
Whether you’re a local or a visitor, it’s important to:
- Understand the risks
- Learn safe tick removal techniques
- Prevent or minimise complications
I’ve personally endured severe illness from improper tick removal -allergic reactions and infections. I created this guide to help you avoid the same.
Major Health Risks from Tick Bites
1. Allergic IgE Reactions (within minutes to 24 hours)
- Local Reaction: Itchy, red, hot skin; raised bump; inflamed area; oozing wound
- Systemic Reaction: Vertigo, weakness, dizziness, muscle aches, light sensitivity, night sweats, low-grade fever, stiff neck, brain fog, nerve tingling, swollen lymph nodes
- Anaphylaxis: Noisy breathing, swollen tongue, wheezing, collapse — requires an EpiPen and emergency care
❗ Improper tick removal increases allergic reaction risk by 85%.
🩺 Immediate Tick Allergy Reaction
An immediate tick allergy reaction is an IgE-mediated immune response to proteins in a tick’s saliva—such as Hol l 5, proteases, cement proteins, and anticoagulants. These proteins are introduced into the host during the tick’s initial attachment. However, if the tick is disturbed, squeezed, or removed incorrectly, it may inject a concentrated dose of these allergens, potentially triggering a severe immune reaction. In some cases ( especialy people with exisiting immune chalenges- allergies or MCAS) , this can escalate into an “immune storm” that lasts for weeks or even months.
🧠 Overlapping Symptoms and Diagnostic Challenges
Symptoms of systemic allegric reaction such as vertigo (wobbly feeling), weakness, dizziness, muscle aches, light sensitivity, night sweats, low-grade fever, stiff neck, brain fog, nerve tingling, and swollen lymph nodes can mimic those of tick-borne infections. This overlap presents a significant clinical challenge, making accurate diagnosis and appropriate treatment more complex.
Tick Bite local allergic reactions

Tick Bite local allergic reactions

Localised allergic reaction that developed into systemic infection

2. Tick Paralysis
Caused by neurotoxins released after 3+ days of tick feeding. Always perform daily tick checks.
- Early Signs: Lethargy, poor balance, loss of appetite
- Neurological Signs: Dilated pupils, slurred speech, facial paralysis, blurred vision, light sensitivity
- Severe Cases: Laboured breathing, slow heart rate, low oxygen. Rarely: myocarditis in children
➡️ Requires emergency medical attention
🩺 Symptoms usually resolve quickly after tick removal
3. Alpha-Gal Syndrome (Mammalian Meat Allergy)
A delayed allergic reaction to mammalian meat.
- Mild to Severe Symptoms: Digestive upset, hives (especially on the torso), or life-threatening anaphylaxis
➡️ If you experience digestive symptoms after a tick bite, ask your GP for a Medicare-covered Alpha-Gal test
🩺 No known cure — requires long-term dietary management
Alpha Gall Reactions:



4. Tick-Borne Infections
- Onset: 5–10 days post-bite (may overlap with allergic symptoms)
- Pathogens: Coxiella, Rickettsia, Babesia, Bartonella, Ehrlichia, Anaplasma, Borrelia, and arboviruses
- Symptoms: Headache, swollen lymph nodes (especially cervical), muscle pain, cognitive issues, moderate-to-high fever (as opposed to low or no fever with allergy), night sweats, fatigue
🔬 Immunosuppressed individuals may not develop a fever, making diagnosis harder.
Erythema migraines ( Bulls eye) is rare in Australia.
🩺 Requires antibiotics and immune support.
Safe Tick Removal – Australian Paralysis Ticks
Critical for reducing the risk of allergic reactions and infections!
✅ Step 1: Kill the Tick While Embedded
Use a -50°C tick freeze spray. Wait for it to detach or carefully remove it using fine-tipped tweezers.
Important: If using fine tip tweezers, grip the head only.
❌ Never squeeze the tick’s body — even if it’s dead.
❌ What Not to Use
- Permethrin (Scabies Cream): Doesn’t kill the tick instantly, increasing irritation and infection risk. Only use in sensitive areas (e.g., eyes, mouth) where freezing spray is not safe.
- Tweezers on a live tick: Greatly increases the risk of allergic reactions.

Common Challenges with Tweezers
- Ticks are often too small to grip
- Frequently embedded in hard-to-reach areas (hair, skin folds)
- Precision is essential — under stress, people often mishandle tweezers and squeeze the tick’s body, causing more harm
Freeze Spray Drawbacks
- Will cause minor skin burn, which typically heal within 3–9 weeks.
- Killed tick still is capable of relaesing neurotoxins if removed incorrectly.
Prophylactic (Preventative) Treatment
1. Homoprophylactic Tick NSW
What is it?
Homeoprophylaxis (HP) is a gentle, non-toxic way to support your body’s natural defenses. Based on homeopathy’s core principle—like cures like—HP uses highly diluted remedies to “educate” your system against specific threats.
Homeopathic Remedy: Ixodes 200C
This remedy I made from a local tick species, carefully potentized so that no physical tick material remains—only its energetic signature. This imprint helps your body recognize the energetic pattern of the tick and its associated pathogens, without any exposure to the actual organism.
How It Works
Rather than force an immune response like vaccines, HP stimulates the body’s innate intelligence. It strengthens awareness and readiness at the energetic level, offering a subtle form of protection that aligns with the body’s natural processes.
Why Choose This?
Made from local ticks for region-specific support
Completely non-toxic and chemical-free
No risk of side effects or suppression
Based on over 200 years of clinical homeopathic use
This is a natural and individualized option for those seeking holistic support in tick-prone areas.
2. Preventative Spray and Clothing
Comin Soon
Post-Tick Bite Treatment
1. Homeopathic Tick Bite Protocol (Days 1–14)
Supports the body in preventing anaphylaxis and tick-borne infections.
- How to take: 3 drops once daily into a clean mouth, at least 10 minutes away from food or drink
- Who needs it: Everyone — even if no visible reaction occurs
Formula: Tick NSW, Aurum arsenicosum, Apis mellifica, Histaminum, Rhus tox, Gelsemium, Lyssin, Borrelia, Ledum- kentian potencies
2. Herbal Tick-Bite Tincture (Days 1–14)
Antimicrobial/ Immune modulating blend specificialy targeting tick borne pathogens.
- How to take: 5 ml, 3x daily in water, ideally on an empty stomach
- Who needs it: High-risk individuals (immunocompromised, elderly, history of tick infections), or anyone seeking extra protection
Individualised Herbal Tincture- based on Stephen Buhners methods.
3. Topical Support: Andrographis + Bentonite Paste (Days 1–5)
Helps draw out toxins, allergens, and supports wound healing.
- How to use: Mix ~3 ml of Andrographis tincture with bentonite clay into a paste. Apply directly to the bite, leave on for 24 hours, and replace daily for 5 days
- Who needs it: Anyone prone to itchy, weeping, or inflamed tick wounds
*6 weeks old tick bite wound, ongoing oozing, one day post Andrographis paste
Post-Tick Bite Treatment
Pharmaceutical Support
Antihistamines
For managing local and systemic allergic reactions.
- OTC H1 blockers: Claratyne (loratadine), Zyrtec (cetirizine), Telfast (fexofenadine)
Doxycycline
- Dosage: 100 mg twice daily for 4 weeks (ILADS standard for Borrelia infections)
Australia doesn’t officially recognise Lyme disease, but local Borrelia species exist.
Important Notes:
- Not everyone needs antibiotics — only take them if symptoms arise
- May impact gut flora — follow gut support protocols
- Some GPs may hesitate due to outdated guidelines
If your GP is reluctant, remind them that Rickettsia and Coxiella are well-documented in Australia and require antibiotics.
Order Tick Bite Kit

A must-have for residents or travellers to tick infected areas!
Includes:
- 30 ml Homeopathic blend – $30
- 200 ml Herbal Immune tincture – $69 ( consultation required)
- 30 ml Andrographis + Bentonite – $25
- Measuring cup and instructions
📦 Shipping: $15 flat rate or free local pick-up (Merimbula or Candelo, NSW)
💰 Save on postage: Order full kit or items individually
Shelf Life:
- Homeopathic: No expiry
- Herbal tinctures: 5 years (store in a dark, cool place)
- Bentonite clay: No expiry
✅ Always keep your kit stocked with freeze spray, tweezers, wound care, and remedies.
TO ORDER
Manual orders only for now.
Send SMS with your full name, address, and items required. Payment via bank transfer.
Order early — postal delays may limit your treatment window.
Bitten by a tick? Need expert advice?
Reach out early — it can make all the difference.